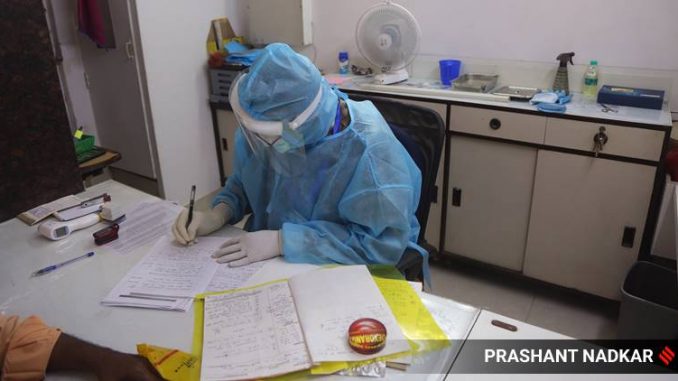
The 5,600 claims, when viewed against the over 1.8 lakh Covid-19 cases, translates to just 3.1 per cent of the individuals who tested positive and had health insurance coverage. (Express photo by Prashant Nadkar)
Covid-19 cases in the country have surged past the 1.8 lakh figure, but less than 10,000 people have so far utilised the health insurance scheme.
According to numbers collated by insurance companies, only 5,600 claims have come to insurers for settlement involving a cumulative amount of Rs 70 crore — this works out to an incurred expenditure of Rs 1.25 lakh, on an average, per policy holder.
The 5,600 claims, when viewed against the over 1.8 lakh Covid-19 cases, translates to just 3.1 per cent of the individuals who tested positive and had health insurance coverage.
On the other hand, only 2,132 people have availed or are now undergoing treatment for Covid-19 (as of May 20) under the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) — the government’s cashless/paperless healthcare access service for poor and vulnerable families — according to data from states that have involved general insurance companies for the scheme.
While the 5,600 claims relate to health insurance policies sold by general insurance or health insurance companies, sources say that in case of many states that have roped in general insurance companies for the scheme, they also include claims relating to Ayushman Bharat.
While Ayushman Bharat covers over 10 crore economically disadvantaged families, there is the CGHS scheme that covers the government employees and the Employees’ State Insurance Corporation (ESIC) scheme for the workers.
The Ayushman scheme is supposed to provide a cover of up to Rs 5 lakh per family per year, for secondary and tertiary care hospitalisation to over 10.74 crore poor and vulnerable families (about 53 crore beneficiaries). Even Covid-19 testing and treatment are supposed to be free for people covered under the scheme.
“Given the weak government health infrastructure, low levels of health insurance penetration and inadequate cover can emerge as a big issue for a large section of the population. Treatment involves isolation ward, ICU admission and ventilator support in critical cases, and can be a costly affair,” said a senior official with a leading general insurance company.
In many cases, the official said, the entire family is testing positive and if they have inadequate insurance cover, then it may be insufficient to cover the medical expense of the entire family.
The average treatment cost in the case of Covid-19 patients is very high in private hospitals. While data on average size of health cover is not available officially, industry insiders say the average size of health cover across the industry is around Rs 2 lakh. Since in the case of Covid, the entire family is at risk, in majority cases the health insurance cover that people have will be inadequate to cover the cost of treatment for the family in case they get infected.
“With no cap on the cost for treatment, whatever few cases being treated in private hospitals are being handed exorbitant medical bills, far surpassing their insurance covers,” the CEO of an insurance company said.
The low number of insurance claims comes even after the government said that empanelled hospitals can use their own authorized testing facilities or tie up with an authorized testing facility.
These tests would be carried out as per the protocol set by Indian Council of Medical Research (ICMR) and by private labs approved/registered by ICMR. Similarly, treatment of Covid-19 by private hospitals will be covered under AB-PMJAY.
According to a McKinsey report on insurance, insurers can support Covid-19 patients by allowing deferred repayments and providing “hospicash” benefits, discounts on co-pays, and so forth.
“Insurers could also launch products with Covid-19 coverage and engage with regulators to expedite the approval process, as well as announce monetary-relief packages for Covid-19 patients,” it said.
The health insurance segment, meanwhile, is the only segment (other than fire) which reported a 6.2 per cent growth in premium income at Rs 5,379 crore in April this year. Health now constitutes 37.9 per cent of the total business of general insurers.
Insurance companies are coming out with their own individual products. Aegon Life Insurance recently announced the launch of ‘life insurance with Covid-19 cover’ for hospitalization expenses up to Rs 1 lakh along with Flipkart.
HDFC Ergo General Insurance Company and Apollo Clinic announced their corporate agency tie-ups to offer insurance products to provide financial security to customers from hospitalisation and treatment expenses.
SBI General Insurance and Yes Bank in partnership with Reliance General Insurance announced the launch of FD+Covid-19 cover for new fixed deposit holders.
source: indianexpress
